It's been about 2 years since the COVID-19 pandemic started. It's been a year since vaccines have been approved. This COVID-19 thing should be over. So why, in hell, am I writing another post about COVID-19?
Unfortunately, it is not over. The US still has more than 1,000 COVID-19 deaths per day. Germany has reported record number of COVID-19 infections in the last couple of weeks. A new virus variant, Omicron, has emerged, which has replaced Delta in regions of Africa, and threatens to do the same in other parts of the world - partly because its many mutations allow Omicron to evade the immune response from vaccinations or previous COVID-19 infections.
In this post, I'll look at some of the things we have learned about Omicron, and from other variants. I'll also look at data from different countries and US states to examine how effective vaccinations are in respect to reducing COVID-19 infections, and in respect to reducing severe COVID-19 cases and deaths.
Finally, I will combine these insights with some basic facts about the human immune response to speculate what will happen in the next years.
Omicron
The Omicron variant of the SARS-CoV-2 virus that has about 50 mutations relative to the original Wuhan strain. What makes Omicron so unusual is that about 30 of these mutations are in the spike protein, which the virus uses to invade human cells; and that there are no closely related strains known.
The first description of the Omicron variant is less than 3 weeks old, so our knowledge about it is still limited. It looks like Omicron first started spreading in the Gauteng province in South Africa in October. In less than 2 months, it become the dominant strain in the Gauteng province, mostly replacing the previously dominant Delta variant. It has also spread to dozens of other countries and US states.
The fast spread of Omicron is an indication that Omicron may be even more infectious than Delta. Reports from the UK, Germany, and other countries indicate that vaccines and previous infections offer only limited protection from infection with Omicron, with protection of 75% or more only seen in persons who recently received a third (booster) vaccine shot, or who received two vaccinations and also had a previous COVID-19 diagnosis.
Currently, there are not enough data available to know how severe COVID-19 caused by Omicron will be. Limited anecdotal evidence suggests that Omicron cases may not be as severe as cases caused by other variants. However, many patients who tested positive for Omicron had been previously infected by other variants, or were vaccinated, which significantly reduces the chances of severe or deadly COVID-19.
COVID-19 Vaccine Effectiveness
A large number of scientific studies from different countries have shown that COVID-19 is effective at preventing COVID-19 infections, but even more effective at preventing severe COVID-19 cases, hospitalizations, and deaths. The RKI in Germany publishes one of the most comprehensive studies on a weekly basis. Germany tracks COVID-19 infections, vaccinations, hospitalizations, and deaths in a central register, which enables tracking the vaccination status for positive cases, hospitalizations, and deaths, and therefore calculating the effect of the vaccinations for each calendar week:
The region shaded in grey at the right side of the graph indicates data from the most recent weeks, which are incomplete due to reporting delays. The data clearly show that vaccinations prevent infections and hospitalizations in all age groups. With careful analysis, this effect can be quantified:
The graphs show that the protection from infection (top left graph) went down slightly over time, from about 85% to about 70%, and then started increasing again due to booster shots in the most recent weeks. The protection from severe outcomes like hospitalization (top right), ICU (bottom left), and death (bottom right) remained higher, generally between 80% and more than 90% for all age groups.Another way to see the effect of vaccinations is by comparing countries, for example the UK and the USA. Let's start with the US (data from https://ourworldindata.org/covid-vaccinations):
The graphs for cases, hospitalizations, and ICU admissions all look quite similar, with the peak in the fall of 2021just slightly lower than the peak in January 2021. However, the summer/fall death peak is somewhat reduced relative to the January peak.
For comparison, here are the graphs for the UK:
Looking at the case numbers in the summer/fall relative to last winter, the trend in the UK was comparable to the US, or even worse, since the case number remained high. However, the second peaks for hospitalizations, ICU, and deaths are all significantly reduced - about 4 x to 9x lower than the peaks numbers last winter. In other words: while the UK has experienced a similar peak in COVID-19 cases in the fall, the increase in severe COVID-19 cases and deaths was several-fold lower than in the US.
The reason for the observed difference can be seen in the vaccination statistics for the two countries:
- Not fully vaccinated (12 years and older)
- Not fully vaccinated (65+):
- US: 12.8%
- UK: <4%
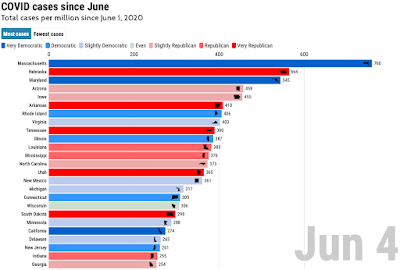
For many southern US states, which were hardest hit by the summer/fall 2021 wave, vaccination numbers are substantially lower than the US averages. For example, more than 20% of the 65+ population in Georgia and Alabama is not fully vaccinated, and the non-vaccinated rate in the 12+ population is above 40% in Alabama (45.3%( Mississippi (44%), Louisiana (41.5%), Tennessee (41.5%), Georgia (41.4%), and Arkansas (41.2%).
The UK data show that vaccinations can cause a substantial reduction in hospitalizations and deaths from COVID-19 if a high percentage of the population (and a very high percentage of the most vulnerable population) is vaccinated.
Variants, Vaccines, and the Immune System
Over the past two years, we have seen a new virus variant replace the previous variants roughly every six months: the original Wuhan strain was quickly replaced by the D614G mutation, which was replaced by the Alpha strain, which was replaced by the Delta strain. In some regions of the world, other variants like the Beta and Kappa strains also temporarily become common or dominant strains.
Each subsequent strain had advantages over the previous strains that helped it become dominant; typically, the newer strains had mutations that made them more infectious, so that they simply spread faster. Some of the later strains also showed some signs of "immune escape", which resulted in increased re-infections, as well as reduced effectiveness of antibody therapies.
What we are seeing is "evolution live": the SARS-CoV-2 virus adapts more and more to its new host, the human body. The speed of this evolution is directly related to the number of infected "hosts" - the more people are infected, the faster the virus will change, becoming better at infecting more people. We have absolutely no reason to believe that this will stop anytime soon; it seems quite likely that Omicron will be replaced by an even "better" variant before the end of the next year, especially given vaccine "hesitancy" in many countries and regions.
Theoretically, vaccines can be adapted for new strains. However, even though data showed that vaccine efficacy was reduced for the Delta variant, no new vaccine that has been modified for Delta has been approved yet. Technically, modified vaccines could be developed within weeks, and manufactured within maybe a couple of months. However, clinical testing for safety and efficacy will likely add several months, and regulatory approval even more time. Additional complications come into play from travel and other restrictions. For example, if traveling requires full vaccination, should a participant in a trial for a new vaccine be allowed to travel before the vaccine he receives is proven to work?
A lot of the research about new variants simply looks at antibodies: how well do antibodies from a vaccinated or previously infected person work against a virus? That's a reasonable question, but there is another reason why we hear a lot about such studies: they are relatively easy to do, and give quick answers. The answers are often condensed down into a single number. For the Omicron variant, for example, reductions by factors of 20 or 40 are often reported.
Interpreting these numbers, however, requires some understanding of the tests that are being done. Typically, the reported number is basically a dilution factor - the "titer" required to inhibit, for example, the ability of the virus to infect cells in the lab. The titer in effect combines two aspects of the antibody immune response: 1. how well antibodies bind to a virus, and 2. how much antibodies are present in the blood. For Omicron, one study reported that a booster shot gives relatively good protection within the first 2 weeks after a booster shot, but significantly less protection after 3 month. The difference here is entirely due to the "how much" aspect of the titer: over time, the concentration of antibodies in the blood goes down (assuming no new infection or vaccination). Typical half lives for antibodies in the blood are in the range of several weeks; so after 3 months, the amount of COVID-19 specific antibodies may have dropped by a factor of 10 to 100.
After a second vaccine shot or a booster shot, the observed antibody titer goes up, which indicates improved protection. This, however, is due to both factors - and increase of the amount of antibodies, and an increase in how well the antibodies bind. Our body is constantly exposed to viruses that want to hijack our cells and multiply - just looking at cold viruses, there are a few hundred different ones out there. All those viruses mutate - some a bit faster than SARS-CoV-2, some slower, but they all change.
To keep up with ever-changing viruses, the immune system has its own "rapid evolution" mechanism. Basically, as the cells that make antibodies against virus multiply and mature, the antibody changes, due to mutations in "hyper-variable" regions in the antibody genes. So a certain fraction of the antibody-producing cells will have mutations that change the antibody a bit, just like a corona virus has mutations that changes its spike protein. This part is just random, but now comes the "clever" part: if a random mutation improves how well an antibody binds to the "antigen", for example the spike protein, then the cells with this mutation will divide faster than "older" cells with not-quite-as-good antibodies.
This process of "antibody improvement" happens every time after a new infection - and after a new vaccine shot. It can improve the binding of antibodies by factors of more than 10 every time, which is one reason why a vaccine with 2 shots tends to work better than a single-shot vaccine. But it can also make the "necessary changes" if a virus has mutated, causing the old antibodies to be less efficient.
Now let's put this all together, and see what that means with respect to Omicron. Let's assume I have had a booster shot recently: my antibodies have now two rounds of improvement after the initial shot, so they will bind the spike protein much better than they would have after the first shot, or even after the second shot. Every person makes different antibodies, partly due to different genes, and partly due simply to chance. The Omicron spike protein looks quite different from the spike protein in the original virus, but if I am lucky, some of my antibodies will still bind modified spike protein well enough. Shortly after the booster, the antibody levels will be high, and my antibodies cover all the spike proteins in all the virus particles that infected me. The virus never stands a chance to multiply to a level where I would have any symptoms.
But more likely, my antibodies recognize the Omicron spike protein, but due to the mutations, don't bind it very well. That means some of the spike proteins remain free of antibodies, and the virus can enter my cells and start multiplying. But some of my antibodies will also do their job, interact with the other parts of my immune system, and start multiplying. As described above, that also means that they'll "check out" some random mutations, and there's a good chance that one of the mutated antibodies binds the Omicron spike protein very well. Maybe it takes a few days for this to happen, and the virus can multiply a bit during that time - enough to give me a sore throat and a mild cough. But after that, my "new and improved" antibodies take over, and the infection is quickly controlled. This is what is often seen in breakthrough infections - the virus initially multiplies and reaches levels similar to what isseen in unvaccinated persons, but then, virus levels drop a lot faster, and symptoms remain lighter.
What I described above partly explains what we see with vaccinations - that they can prevent infections, but are even better at preventing severe COVID-19. In fact, the observed protection against several variants, including Delta, was better than what would have been expected from antibody-binding studies. The explanations above are, of course greatly simplified. For example, I did not go into the role of the "second arm" of the immune system at all, the T-cell mediated immune response; nor did I mention the effect of repeat immunizations on memory cells (just like learning, repeating usually helps). But the data we have so far are quite clear: vaccines protect; more shots protect better; and more recent is better. So if you qualify for a booster, but have not gotten one yet, go get one!
Time for Coronas
So, the virus causing COVID-19 is here to stay, and will likely keep mutating, perhaps faster than vaccines can keep up. Over time, it is very likely that infections become less dangerous. We are seeing this already in the UK, where case fatality rates have fallen by at least fourfold, and in other countries with high vaccination rates. We will also soon have effective medications that can be taken in pill form, based on similar mechanisms as the protease inhibitors that have worked so well for HIV infections.
We have seen that protection against COVID-19 seems to fade over time, and that multiple exposures to the vaccine and/or infection increase protection. Given how widespread COVID-19 infections are, and the observed seasonality, we will keep seeing waves of COVID-19 infections for years to come. It is quite likely that the severeness will go down over time, if our immune systems are exposed to the virus or a vaccine on a regular enough basis. After three vaccine shots, I'll be happy to expose myself to "natural exposure" again more frequently - time for Coronas, the Mexican kind (or perhaps a local brew instead). So I do hope that this will indeed be my last post on the subject of COVID-19.
I'll finish with a couple of graphs that illustrate the danger of declaring "it's over" too early - something that a lot of states and countries have done. Here's a look at the ICU usage in Florida:
A comparison of excess death rates (in percent relative to expected deaths) for Texas and Massachusetts:
Those are graphs based on all death certificates submitted to the CDC by local authorities, so there is no political meddling possible. The data for the last few weeks are incomplete. The CDC data show 95,147 excess deaths for Texas, 70,138 excess deaths for Florida, and 11,333 excess deaths for Massachusetts (which has about 1/3rd of the population of Florida, and 1/4th of Texas).