This post looks into several important new insights into COVID-19 that were described in recent publications. I will also look at what this means for us - why it is very important to stick to social distancing and related prevention measures. It's long, so I'll give you a
Short version
- If you get exposed to 500 COVID-19 virus particles, you'll probably get infected. That one "infectious dose".
- If you're infected, you probably don't know it. You'll be most likely to infect others before you have any symptoms.
- When talking, an infected person emits about 500 infectious doses per hour, which would theoretically be enough to infect 500 others. Talking loudly, singing, and yelling increases to 2,500 infectious doses per hour. There are many examples of one person infecting dozens of others.
- The virus particles are in aerosol droplets that can remain airborne for up to several hours, and therefore accumulate indoors.
- Do the right thing.
Long version
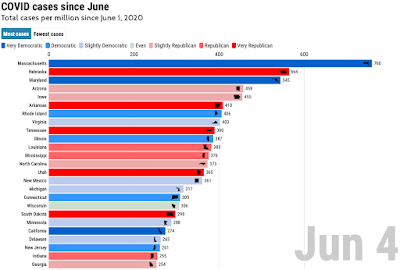
Let's start with a graph that tells us a lot about CVID-19 infections:
This is from a in-depth study of infections in Austria. The scientists used a combination of contact tracing and DNA sequencing to study how exactly the COVID-19 virus was passed from one patient to the next. To get this information, they looked at new mutations that are always present in a subset of virus particles in each infected person, and compared these to the mutations found in others a patient had expected. This allowed the scientists to estimate how many virus particles (or virions) had been passed from one patient to the next - the "bottleneck size" in the graph above.
The results indicate that in many cases, a couple of thousand virions were passed on during an infection. However, a similar number of patients had been infected by a lower number of virus particles, between 20 and 200. In one of the infections studied, the transmission only involved fewer than 10 virions - possible as few as two.
The science behind these results is, in my opinion, pretty cool. But perhaps I am biased, since is is closely related to the type of research for which I have developed commercial software for the last 20 years. Anyway, the study was a collaboration of more than 30 scientists from several top level labs in Vienna and at Harvard, the MIT, and the Dana-Farber Cancer Institute.
The results show what many virologists so far only had suspected: that COVID-19 infections are usually caused by several hundred to thousand virus particles that are somehow transferred from an infected person to another person. Infections can also happen at a lower number of virus particles, but that appears to happen only rarely.
The data indicate that the "independent action hypothesis" of viral infections applies to COVID-19. It basically states that each virus particle that enters your body has a small chance of establishing an infection and causing disease (or, for COVID-19, an asymptomatic infection that can nevertheless infect others). The more virus particles enter your body, the higher the chance that you're getting sick. Here is a graph that illustrates this relation:
An important concept here is the "infectious dose". That is the number of virus particles that has a 50% chance of creating a "successful" infection. For COVID-19, that number seems to be somewhere around 500. We don't know the precise number - it could be 200, or it could be 1000, but it is very unlikely that it is below, say, 100 or above, say, 5000. Note that below this dose, the chance of infection is not zero, but rather declines in a near-linear fashion.
A bit simplified, the "infectious dose" (ID) means this: if you get infected with this many virus particles, the chance that you'll get COVID-19 is slightly higher than the chance that the COVID-19 virus fails to establish itself in our body. Get more than the ID, and you'll most likely get COVID-19; get less, and your chances of walking away healthy are better. That raises the question:
What are the chances of receiving an "infectious dose" of the COVID-19 virus?
To answer this question, we first need to look at how someone with an active COVID-19 infection passes the virus on to someone else. We know that saliva and lung fluids of an infected person can contain a lot of virus particles - a typical number is 100 million virions per milliliter. That's about 200 thousand infectious doses (or, short, IDs)! Some of this fluid, and the virus particles in it, is emitted as droplets of various sizes when a person coughs, sneezes, speaks, sings, or just breathes - but the number and size of these droplets depends a lot on what exactly a person is doing. Coughing and sneezing can produce the largest droplets - perhaps the word "gross" fits (especially if you speak German). But we now know that most COVID-19 transmissions happen before symptoms appear, when coughing and sneezing cannot play a role. If you're interested in the details, I suggest you check this preprint and the references in it. I'll just summarize the results from a different study that combined knowledge about particle sizes, viral loads, and actual transmissions in five super-spreader events for different activities:
- Breathing: ~10 IDs / hour (5-10-fold higher during hard exercise)
- Talking: ~500 IDs / hour
- Singing: ~2,500 IDs / hour
Yelling is similar to singing, and loud speaking in between talking and singing. Note that these particles are in aerosols that can remain airborne for up to several hours.
Now remember that you want to avoid getting anywhere close to just one ID (that is 500 virus particles). If you are sitting really close to someone, you end up "sharing breath" with that person - a significant percentage of the air he breathes out you breathe in. If you're close enough to someone in an area with little ventilation, you could "collect" one ID within a couple of hours, even if he is just breathing! Fortunately, "breath sharing" drops very quickly as the distance between two persons increases, and a distance of four feet or more is usually sufficient to reduce your "collection" to a small fraction of one ID per hour. But remember that this only reduces your risk of infection - it does not eliminate it!
But as you can see from the list above, things get a lot worse when talking or singing. When breathing, the droplets you emit are very small; but when talking, yelling, or singing, the droplets are a lot bigger. A 10-fold larger droplet has 1000-fold more volume, so a given number of droplet can contain 1000-fold more virus particles. But most of the "large" droplets generated by talking are still so small that the water in them evaporates very quickly in normal room air, shrinking the particles to sizes that can remain airborne for a long time ... just waiting for you to breathe them in.
With this in mind, let's consider going out to dinner with a couple of friends we have not seen in a while. We'll go to a restaurant and share a nice booth between four people, not knowing that one of them had gotten infected with COVID-19 a few days ago, and is now shedding the virus at a high rate. Someone is talking all the time, but we're nice and take turns, so the infected person is talking just one fourth of the time. After an hour, though, he has emitted about 500 / 4 = 125 "infectious doses". Let's say the booth is about 2 x 2 x 2.5 meters, or about 10 cubic meters. Without any air exchange, the concentration of infectious doses in the both air would be 125 IDs / 10 cubic meters, or 12.5 IDs / cubic meter. We breath about half a cubic meter of air per hour - so everyone on the table would have been exposed to about 6 infectious doses of the virus, making it very likely they'd get infected.
The unrealistic assumption in our example is that there is no air exchange. In reality, ventilation in typical building creates exchanges the air about 4-10 times per hour. That would drop the virus concentration in our booth by a comparable amount. But it would still leave each of the three uninfected people on the table "collecting" about 1/2 to one infectious dose, meaning it would be almost certain that at least one person would get effected.
So far, we have looked at two parts of the "infection equation": how many virus particles are needed to infect someone with COVID-19, and how many virus particles (or infectious doses) an infected person "emits". But we also need to look at a third part: when an infected person emits virus particles, relative to when they were infected and to when they experience symptoms.
Wrong person, place, and time
While there are still plenty of uncertainties and gaps in our knowledge of COVID-19, scientists from all over the world have collected and published a lot of data that can guide our efforts. In some important aspects, COVID-19 is very different from other infections like influenza. Two of these aspects are the highly variable incubation time and the high variability of symptoms, which includes the frequent complete absence of symptoms. Other diseases progress is a well-defined fashion, for example a symptom-free incubation period of 3-4 days, following by a symptomatic period, with the highest infectivity a few days after first symptoms.
But for COVID-19, the incubation period can vary between 2 and 14 days, and multiple studies have shown that many transmissions occur before a patient has any symptoms, and from persons who never develop any symptoms, or only light, non-specific symptoms. In many super-spreader events, where one infected person infected dozens of others, the "super-spreader" had no or only mild symptoms. Based on these and other data, scientist now think that an infected person is most likely to infect others in just a relatively short period; in symptomatic patients, this is just before symptoms appear.
If an infected person has close contact with many others during this short period of "maximum infectivity", he can infect many of his contacts in a short time - often within an hour or two. Being at the wrong place at the wrong time, and sharing space with the wrong person, makes it extremely likely to get infected. With many contacts, many get infected, as the graph below (from this publication) shows:
What does that mean? Let's go back to our "restaurant with friends" example from above. Since many COVID-19 transmissions happen before symptoms appear, it means very little that our friends do not have any COVID-19 symptoms. The high variability in incubation times means that they could have been infected just a couple of days ago, or two weeks ago, and just now reach their maximum infectivity period, during which we will get infected if we are close to them for an hour. But given the high shedding of infections virus particles when talking, it might not even be our friends who infect us - it could be someone sitting a couple of tables away, or someone who had our booth before us. Sure, the risk of infection is highest when you are close to an infected person, so you should keep at least a 6 ft distance from others whenever possible. But aerosol particles can quickly travel much farther than 6 ft, and any air flow from ventilation can help distributing them. With incubation times as short as 2 days, even someone who just was tested for COVID-19 two days ago may be infectious now.Break the infection chain. It's not just about you - it's about the ones you infect, and they ones they infect, and so on.
Keep your distance.
Wear your face mask. They work. We know why they work. The better it fits, the better it works - especially at protecting you. Perhaps a 20 or 50% lower chance of getting infected does not mean much to you - but if everyone wears masks (and follows other guidelines), it will drop transmissions by 50%, and the epidemic will "just go away". It's not political. It public health, consideration for others - and the best way to get the economy back on track. Just ask Australia.