This page describes a systematic pattern of misrepresenting information about COVID-19 by officials in Florida. These officials include the governor Ron Desantis, the governor's spokesman Fred Piccolo Jr., Florida's Surgeon General, Dr. Scott A. Rivkees, and Republicans in the Florida House.
A Red Flag: Is COVID-19 Becoming More Deadly in Florida?
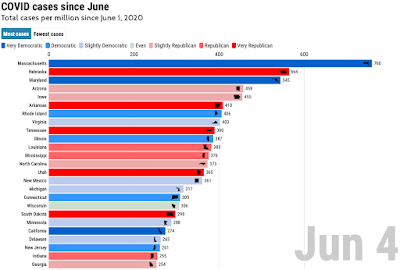
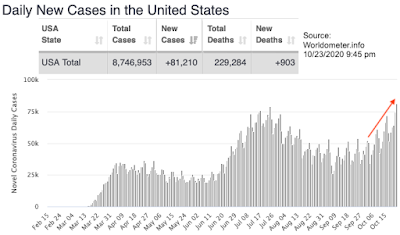
What started my investigation was a strange observation: based on reported COVID-19 confirmed case numbers and deaths, it appeared that COVID-19 is becoming more deadly in Florida than it has been during the summer peak. One way of looking at this is by looking at the relation between reported case numbers and reported death rates; since deaths are typically delayed by several weeks relative to test results, I am comparing death rates to case rates two weeks earlier, using 2-week averages for both deaths and cases:
While the time-adjusted case fatality ratio (CFR) for the US remained almost constant for the US between July and October, it increased from about 1.3% to about 4% for Florida. This peculiar increase prompted me to look for possible explanations.
The Florida COVID-19 Dashboard: How to Understate COVID-19 Deaths
One of the first stops was Florida's official COVID-19 dashboard. The graphs on the right side that depict cases and deaths are interesting:
The top graph shows the new cases, which show an increase over the last month. The bottom graph shows COVID-19 deaths, and the immediate impression is that things must be getting a lot better - the graph shows a clear downward trend in deaths! Wonderful - but in direct contradiction to the increasing fatality rates we had seen in the previous figure. What gives?
The first hint comes from the title "Resident Deaths by Date of Death". That seems reasonable enough - until you read the fine print: "The Deaths by Day chart shows the total number of Florida residents with confirmed COVID-19 that died on each calendar day (12:00 AM - 11:59 PM). Death data often has significant delays in reporting, so data within the past two weeks will be updated frequently."
The key here is that "death data often have significant delays in reporting". That means that the numbers for the last several weeks understate the actual death substantially; the number for the last few days show only a small fraction of the deaths that actually occurred. But rather than stating this clearly, the fine print states that data "will be updated frequently". Perhaps understating the actual death toll may be a bad thing, but updating frequently must be a good thing, right?
But the Florida government had a reason to choose the "death by day" reporting: it will always show a positive trend in deaths, since there will always be fewer cases for the last few days. Anyone who looks at the graph without reading and understanding the fine print will always conclude that the COVID-19 situation in Florida is improving. Always. And who reads the fine print?
For an example, we can use the screen shots of the Florida COVID-19 dashboard that the COVID Tracking Project has captured. Here is what the death graph looked on 8/2/2020:
 |
Death by day 8/2/20
|
For comparison, here is what the graph looks like when plotting the number of new death reported:
That's a very different picture for the last two weeks of July! If we look at the screenshot of the Florida dashboard from 8/15, it gives a very different picture for these weeks:
 |
Florida dashboard as of 8/15
|
Note that the cases around 7/20 now hover around 160 per day, instead of the 120 per day as reported on 8/2. For the beginning of August, we now see around 140 cases per day; two weeks later, this increases to 180 per day.
The bottom line is that the "By day of death" graph on Florida's COVID-19 dashboard will never show an accurate picture of the actual trends in recent weeks. It will always understate deaths for the last 2 weeks substantially, and show a decline of deaths in the most recent days. Given the observed reporting delays, the only apparent purpose of the death graph on Florida's COVID-19 dashboard is to mislead.
Even worse, the graph creates an incentive to delay the reporting of COVID-19 deaths. Early in the COVID-19 epidemic, Florida's board of medical examiners published data about COVID-19 deaths directly. However, when the government noticed that the numbers reported by the medical examiners where higher than the numbers reported by the state, the health department stopped the release of the medical examiner's list. Afterwards, only numbers released by the Florida Department of Health were available, whenever the department chooses to include a deaths. When deaths are added with a 2-week delay, as was typical in the summer, it would help to create the impression that the worst problems were in the past. If a death was added more than 30 days after it happened, it would never show in the death graph on Florida's COVID-19 dashboard.
This created a strong incentive to delay death reports in Florida for anyone who wanted to downplay the severity of the COVID-19 epidemic. As a result, the reporting delays increased substantially since the summer:
But while the delayed reporting was welcome when it reduced the number of reported COVID-19 deaths in the summer, it is now creating a problem: eventually, the death have to be reported!
Killing Two Birds With One Stone: "Investigate All COVID-19 Deaths!"
On October 21, Florida's Surgeon General, who had remained surprisingly quiet during the COVID-19 epidemic up to this point, issued a
press release stating that all COVID-19 fatalities reported to the state will be subject to a "thorough review". In addition to criticizing that some reports were more than 30 days late, he focused on 5 cases where more than three months had elapsed between the COVID-19 diagnosis by PCR test and the eventual deaths.
The issue was quickly picked up by governor DeSantis' spokesman Fred Piccolo Jr., who
stated:
"What is different about the deaths, is that the health department was
finding people who were admitted as positive as far back as March or
April and who passed away in August or September or October. Is that a
COVID death?”
Looking at the data in the Surgeon General's press release shows that Piccolo is stretching the truth beyond the breaking point. Questioning if someone who was diagnosed in March and died in October really died of COVID-19 seems reasonable, right? But the earliest test date listed by the Surgeon General was from June, not March or April - three months later. The longest elapsed time between test report and death was 111 days. While this is still a long time, it is shorter than times that have been reported for people who recovered from COVID-19, as a quick Google search shows:
- A patient in North Carolina was released after 137 days in the hospital. Her complications which were directly caused by COVID-19 included a heart attack and kidney and lung failure.
- Two men in Georgia were in the hospital for COVID-19 for more than 4 months. One of the two was released, the other is still in the hospital.
- A 35-year of woman in the UK was treated for 141 days in the hospital, which included 105 days on the ventilator.
The last case is interesting because the treatment happened in a hospital run by UK's National Health Service - a public health system that Republicans typically describe as "socialist".
Those are just some random samples from a quick internet search, and all of the listed patients survived. Scientific studies show that
survivors typically spend less time in hospitals than patients who die; other studies report very long hospital stays, for example three patients with
more than 50 days in a hospital in one early study from China (as well as two more patients who still were in the hospital after 37 days). Other studies show that hospital stays in the US tend to be longer than in China, and that a significant fraction of patients stay in hospital care for more than 40 days. Some patients get admitted to the hospital for COVID-19 multiple time. In one case in Belgium, DNA sequencing proved that a patient had been infected on two separate occasions from different people; this patient died from the second infection.
These examples show that there is plenty of both anecdotal and scientific evidence of patients who require hospital treatments for several months, and that a small number of cases with a large time between diagnosis and death is therefore not suspicious. It is very likely that the investigations will come to the same conclusions, although it is extremely unlikely that the Florida government would announce such conclusions.
The Pattern: Create Doubt About COVID-19 Deaths
The Surgeon General's press released discussed above is just one of many examples where Republican politicians in Florida try to create doubt about the true number of COVID-19 deaths. A recent example is a "Florida House report" commissioned by Republican House Speaker Jose Oliva. The report says that "60% of death certificates issued for state residents whose deaths were attributed to COVID-19 had reporting errors and most were filed by medical examiners". It speculates that this "may be inflating the COVID-19 death toll by 10%".
Phased differently, the results could be phrased as "a close investigation looking for problems has found that 90% of the reported death are definitely due to COVID-19, with the remaining 10% possibly being due to COVID-19 or some other cause". But instead, the House Speaker, who has no medical background, talks about "compromised data".
Note that the reporting about the issue starts with casting doubt on 60% of the death certificates. It is likely that many readers will remember this particular number, and few will remember than in reality, at most 10% of the death certificates are questionable with respect to COVID-19.
Another example of the "cast doubt" strategy is governor DeSantis' mentioning of the death of a motorcyclist who had tested positive in an accident, and who was initially included on Florida's list of COVID-19 related deaths. However, even before governor DeSantis made the statement in an interview on July 20, this case had already been removed from the reported death counts. Nevertheless, this example is very "sticky", and comes up frequently in conversations with COVID-19 deniers.
The Reality: Florida Reports Less Than 3 Out Of 4 COVID-19 Deaths
The is a simple number that really determines how deadly the COVID-19 epidemic is: the number of people who die in addition to the number who would die in a typical year without COVID-19. This number, called "excess deaths", can easily be looked up based on death certificate data that all states submit to the CDC, and which the CDC publishes on its web site.
Based on spreadsheets last updated on 10/21/2020, and looking at actually submitted death certificates from the weeks ending between 3/7 and 9/19/2020, we can compare the excess deaths to the number of death certificates that listed COVID-19 as a cause of death:
During these roughly 6 months, the number of excess deaths in Florida was 21,263 (note that this number will go up slightly in the next few months, since some deaths certificates are submitted with delays up to a year). Of these, 14,795 death certificates listed COVID-19 as a cause of death. This is about 69.6% of the excess deaths. The graph above shows that excess deaths and COVID-19 deaths follow the same pattern, which strongly indicates that the vast majority of excess deaths is most likely caused by COVID-19, and not some other cause like violence or suicide.
The data for excess death calculations are readily available. Excess death analyses have been published on many web sites, including the Financial Times and Our World In Data. Several scientific studies have analyzed excess mortality in the US, including a study recently published by the CDC. There is world-wide agreement on using excess mortality analysis to determine the impact of epidemics.
The result of excess death analysis for Florida is clear: the current process fails to correctly identify COVID-19 as a cause of death in 3 out of 10 cases. The COVID-19 reporting problem that Florida has is one of under reporting, not of over reporting. This could be addressed by requiring COVID-19 tests and, if necessary, autopsies for any deaths where COVID-19 cannot be excluded by clear evidence.
Just don't wait for the governor or state Republicans to suggest that.